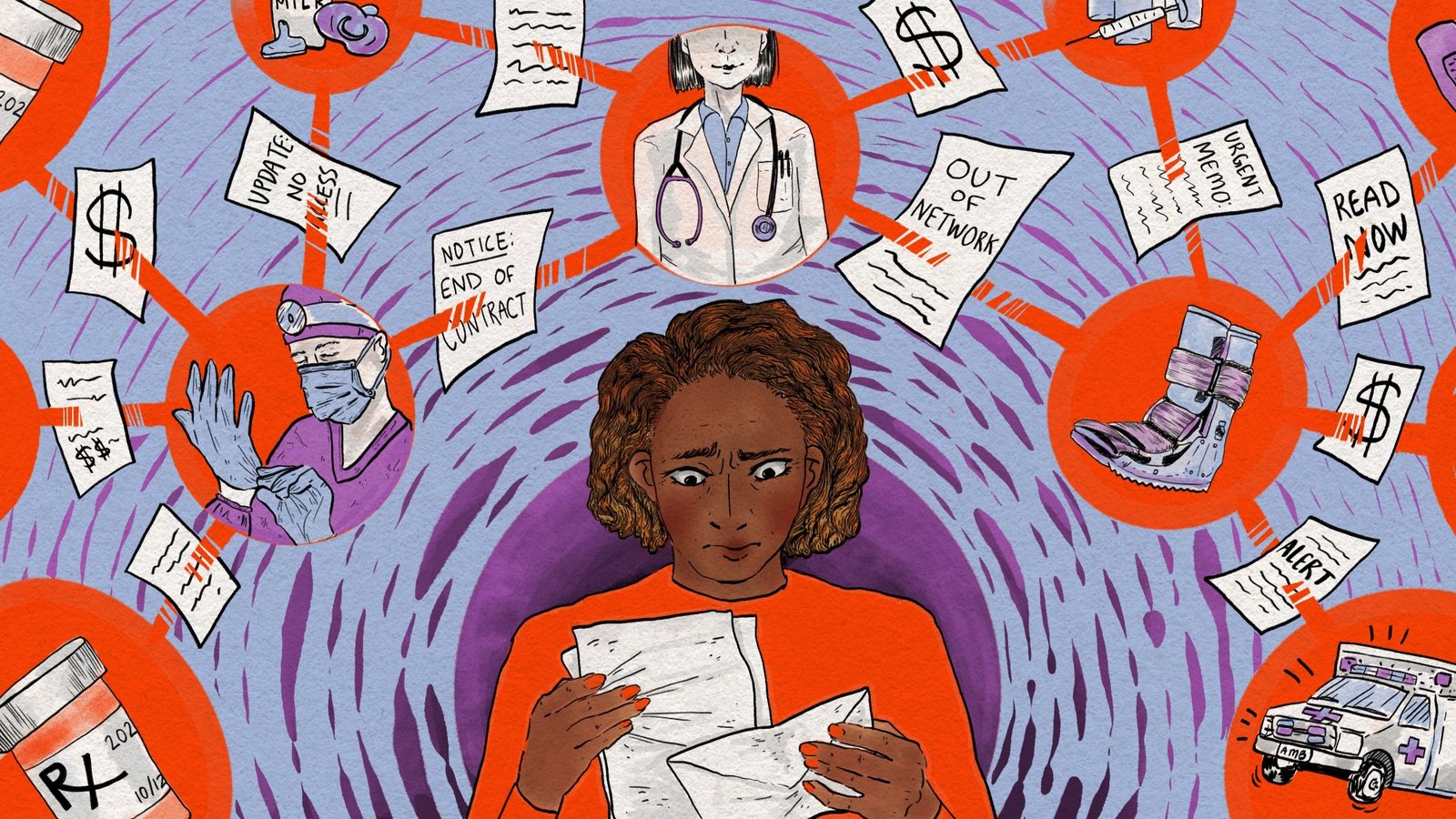
Off the grid and on your own? What to do if the insurance company drops your doctors?

When a Missouri mother’s health insurance company couldn’t reach an agreement with her hospital, most of her doctors were suddenly out of network. She wondered how she could cover the costs of her children’s care or find new doctors. "For a family of five,… where do we start?"
Amber Wingler, 42, from Columbia, Missouri
Last winter, Amber Wingler began receiving a series of increasingly urgent letters from her local hospital in Columbia, Missouri, informing her that her family’s health care might soon be upended.
MU Health Care, where most of her family’s doctors work, was mired in a contract dispute with Wingler’s insurance company, Anthem. The current contract was due to expire.
Then on March 31, Wengler received an email alerting her that Anthem would remove the hospital from its network the next day. It left her reeling.
"I know they go through contract negotiations all the time, but it doesn’t seem like the bureaucracy won’t affect us. I’ve never been kicked off the grid like this before," She said.
The timing was terrible.
Wengler’s 8-year-old daughter, Cora, had unexplained problems with her intestines. Waiting lists to see many pediatric specialists for diagnoses, from gastroenterology to occupational therapy, were long — ranging from weeks to more than a year.

(In a statement, MU Health Care spokesman Eric Mayes said the health system is working to make sure children with the most urgent needs are seen as quickly as possible.)
Suddenly, Quora’s specialty visits were off the grid. At a few hundred dollars apiece, the out-of-pocket cost would have quickly added up. The only other pediatric specialists Wengler found in-network were in St. Louis and Kansas City, both more than 120 miles away.
So Wingler delayed her daughter’s appointments for several months while she tried to figure out what to do.
Nationally, contract disputes are common with more than 650 hospitals in a public dispute with an insurance company since 2021. become more frequent As hospitals brace for nearly $1 trillion in cuts in federal health care spending outlined by President Donald Trump Signature legislation It was signed into law in July.
Patients caught in a contract dispute have a few good options.
"There is an old African proverb: When two elephants fight, the grass gets trampled. Unfortunately, in these cases, patients are often weedy," said Caitlin Donovan, a senior director at the Patient Advocate Foundation, a nonprofit that helps people get health care.
If you’re feeling overwhelmed by a contract dispute between your hospital and your insurance company, here’s what you need to know to protect yourself financially:
1. “Out of network” means you’ll likely pay more

Insurance companies negotiate contracts with hospitals and other medical providers to determine the prices they will pay for various services. When they reach an agreement, the hospital and most of the providers who work there become part of the insurance company’s network.
Most patients prefer to see providers who are… "inside the network" Because their insurance picks up some, most, or even all of the bill, which could be hundreds or even thousands of dollars. If you see an out-of-network provider, you could be on the hook for your entire tab.
If you decide to stick with your familiar doctors even though they are out-of-network, consider asking about getting a cash discount and your hospital’s financial assistance program.
2. Disagreements between hospitals and insurance companies are often resolved
When brown university health policy researcher Jason Buxbaum He said he examined 3,714 non-federal hospitals across the United States and found that about 18% of them had a public dispute with an insurance company at some point from June 2021 to May 2025.
Eventually, about half of those hospitals dropped out of the insurer’s network, according to Buxbaum’s preliminary data. He added that most of these breakups are eventually resolved within a month or two. So it’s very possible for your doctors to return to network, even after separation.
3. You may qualify for an exception to keep costs lower
Some patients suffer from Serious or complex cases You may be eligible for an extension of in-network coverage, called continuity of care. You can apply for this extension by contacting your insurance company, but be aware that it can be a long process. Some hospitals have even set up resources to help patients apply for this extension.

Wingler administered this challenge to her daughter, spending hours on the phone, filling out forms and sending faxes. But she said she doesn’t have the time or energy to do that for everyone in her family.
"My son was undergoing physical therapy" She said. "But I’m sorry my friend, just do your exercises that you have already done. I’m not fighting to get coverage for you either when I’m already fighting for your sister."
It’s also worth noting that if you’re dealing with a medical emergency, for most emergency services and hospitals Can’t charge more of patient rates within the network.
4. Switching your insurance company may need to wait

Maybe you’re considering switching to an insurance company that covers your favorite doctors. But beware: Many people who choose their own insurance plans during the annual open enrollment period remain enrolled in their plan for a year. Insurance contracts with hospitals are not necessarily on the same schedule as yours "Plan year."
Some life events Such as getting married, having a child, or losing a job can qualify you to change insurance outside of the annual open enrollment period, but having your doctors drop out of the insurance network is not a qualifying life event.
5. Doctor shopping can be time consuming
If the split between your insurance company and hospital seems permanent, you may want to consider finding a new list of doctors and other providers in network with your plan. Where to start? Your insurance plan likely has an online tool where you can search for in-network providers near you.
But be aware that making the switch may mean waiting to establish a patient with a new doctor and, in some cases, traveling a reasonable distance.
6. It’s a good idea to keep your receipts
Even if your insurance and the hospital don’t reach an agreement before their contract expires, there’s a good chance they will enter into a new agreement.
Some people decide to postpone appointments while they wait. Others keep their appointments and pay out of pocket. Keep your receipts if you do this. When insurance companies and hospitals do reimburse, the deals are often outdated, so appointments you paid for out of pocket may be covered.
The end of the ordeal

Three months after the contract between Wingler’s insurance company and the hospital expired, the two sides announced they had reached a new agreement. Wengler joined the throng of patients rescheduling appointments they had missed during the ordeal.
In a statement, Jim Turner, a spokesman for Anthem’s parent company, Elevance Health, wrote: "We approach negotiations with a focus on fairness, transparency, and respect for all those affected."
MU Health Care’s Maze said: "We realize how important timely access to pediatric specialty care is for families, and we are truly sorry for the frustration some parents felt in scheduling appointments following the resolution of our Anthem contract negotiations."
Wingler was happy that her family could see her providers again, but her relief was tempered by her determination not to be in the same situation again.
"I think we’ll be more serious when open enrollment comes," Wengler said. "We never bothered looking at our outside coverage before because we didn’t need it."
The Health Care Helpline helps you overcome health system barriers between you and quality care. Send us your tough question and we might turn to a political investigator to solve it. Share your story. The crowdsourcing project is a co-production between NPR and KFF Health News.
KFF Health News It is a national newsroom that produces in-depth journalism on health issues and is one of the core drivers of KFF.
Copyright 2025, KFF Health News












Post Comment